As its name implies, pseudogout has many of the same symptoms as gout, including the sudden onset of severe pain, swelling, warmth, and redness in a joint.
Pseudogout can affect any joint. It is most likely to affect the knee, wrist, or large knuckles of the hand (metacarpophalangeal joints), and may also involve the hip, shoulder, and spine. 1 Genetic and Rare Diseases Information Center, National Institute for Advancing Translational Sciences. Chondrocalcinosis 2. Last updated January 12, 2018. Accessed August 4, 2020. https://rarediseases.info.nih.gov/diseases/1292/chondrocalcinosis-2 , 2 Slobodonick A, Toprover M, Pillinger M. Crystal Arthritis. In: Efthimiou P, ed. Absolute Rheumatology Review. Springer Nature Switzerland AG; 2020; chap 15. Accessed September 15, 2020. https://doi.org/10.1007/978-3-030-23022-7_15 Unlike gout, pseudogout rarely affects the big toe. 2 Slobodonick A, Toprover M, Pillinger M. Crystal Arthritis. In: Efthimiou P, ed. Absolute Rheumatology Review. Springer Nature Switzerland AG; 2020; chap 15. Accessed September 15, 2020. https://doi.org/10.1007/978-3-030-23022-7_15
What Is Pseudogout?
Pseudogout occurs when microscopic calcium pyrophosphate crystals accumulate in a joint and trigger an immune system response. Doctors may refer to pseudogout as calcium pyrophosphate deposition (CPPD) or acute calcium pyrophosphate crystal arthritis (acute CPP crystal arthritis).
See What Is Calcium Pyrophosphate Crystals Deposition (CPPD)?
Without treatment, an episode of pseudogout can last weeks or months. 2 Slobodonick A, Toprover M, Pillinger M. Crystal Arthritis. In: Efthimiou P, ed. Absolute Rheumatology Review. Springer Nature Switzerland AG; 2020; chap 15. Accessed September 15, 2020. https://doi.org/10.1007/978-3-030-23022-7_15 Successive episodes may last longer and/or may affect more joints.
Pseudogout is less common than gout and osteoarthritis, and can be mistaken for gout, osteoarthritis, or rheumatoid arthritis. The initial treatments for these conditions are similar, so an incorrect or delayed diagnosis will not necessarily delay pain relief.
How Is Pseudogout Different than Gout?
Doctors sometimes refer to pseudogout and gout as crystal-induced arthropathies, which simply means they are joint diseases caused by microscopic crystals.
The primary difference between gout and pseudogout is the type of crystals that cause symptoms:
- Pseudogout is caused by calcium pyrophosphate dihydrate crystals, often referred to as calcium pyrophosphate crystals or CPP crystals.
- Gout is caused by monosodium urate crystals, often referred to as uric acid crystals.
Unlike pseudogout, gout is often linked to alcohol consumption, diet, excess weight, and taking certain medications.
Researchers have known about calcium pyrophosphate crystals for decades but still do not fully understand why some people who have them experience pseudogout episodes and others do not.
In This Article:
- All About Pseudogout - Symptoms, Diagnosis, Treatment
- Pseudogout Symptoms
- Pseudogout Causes
- Pseudogout Diagnosis
- Pseudogout Treatment
What Is Calcium Pyrophosphate Deposition (CPPD) Disease?
Pseudogout is just one form of calcium pyrophosphate deposition (CPPD) disease. A person who has calcium pyrophosphate crystals (CPP crystals) in one or more joints is considered to have CPPD disease.
Experts estimate 7% to 10% of the population has some form of CPPD disease.2 The typical forms of the disease include:
-
Acute CPP crystal inflammatory arthritis (pseudogout)
This form of CPPD causes an immune response that results in sudden, severe pain, swelling, redness, warmth, as well as other possible symptoms. It typically affects fewer than 5 joints.
-
Chronic CPP crystal inflammatory arthritis
This form of CPPD triggers a less extreme immune system response than pseudogout. It results in mild, chronic, dull pain with some swelling and redness.
Chronic CPP arthritis can affect one to many joints. It is most likely to affect the wrists, shoulders, large knuckles, or feet. The symptoms are often similar to osteoarthritis or rheumatoid arthritis (pseudo-RA). 2 Slobodonick A, Toprover M, Pillinger M. Crystal Arthritis. In: Efthimiou P, ed. Absolute Rheumatology Review. Springer Nature Switzerland AG; 2020; chap 15. Accessed September 15, 2020. https://doi.org/10.1007/978-3-030-23022-7_15
-
Non-symptomatic CPPD disease
Calcium pyrophosphate crystals may be present in a joint but cause no pain. Many people have no symptoms and are not aware they have CPPD.
In fact, one clinical study 3 Viriyavejkul P, Wilairatana V, Tanavalee A, Jaovisidha K. Comparison of characteristics of patients with and without calcium pyrophosphate dihydrate crystal deposition disease who underwent total knee replacement surgery for osteoarthritis. (Abstract only.) Osteoarthritis Cartilage. 2007 Feb;15(2):232-5. Epub 2006 Oct 10. PubMed PMID: 17045495. found that 54 of 102 patients (52.9%) undergoing total knee arthroplasty had evidence of calcium pyrophosphate crystal deposits in their joint tissue. Only 1 of the subjects was previously aware they had crystals in their knee joint.
People who have no symptoms do not need any medical treatment. There is no pain or inflammation to treat, and there is no way to remove the CPP crystals.
While pseudogout is the primary focus of this article, chronic CPP crystal inflammatory arthritis is also discussed.
How Does CPPD Disease Cause Symptoms?
While experts have known about calcium pyrophosphate crystals for decades, research has yet to uncover exactly why some people develop CPPD disease or why some people experience symptoms and others do not.
Many experts suggest the following steps occur:
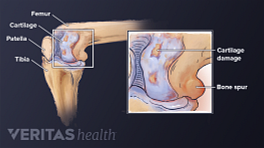
- Calcium pyrophosphate crystals are produced within a joint's cartilage. They can form when too much inorganic pyrophosphate (PPi), a compound naturally found in cartilage, accumulates. The excess PPi binds with calcium, leading to the formation of crystals.
This cascade of events may occur because of:
- Faulty metabolism within the cartilage itself 4 Pritzker KP. Crystal deposition in joints: prevalence and relevance for arthritis. J Rheumatol. 2008 Jun;35(6):958-9. PubMed PMID: 18528950.
- A more general metabolic disorder that is not isolated to cartilage. (A systemic metabolic disorder affects the body’s ability to process and absorb nutrients.)
- An endocrine disorder, which affects the body’s ability to produce hormones.
- As CPP crystals continue to form, they accumulate in the cartilage.
- The excess CPP crystals may be released from the cartilage. This release may happen if the cartilage is disturbed through normal wear-and-tear, an injury, trauma, surgery, or infection. 5 Ivory D, Velázquez CR. The forgotten crystal arthritis: calcium pyrophosphate deposition. Mo Med. 2012 Jan-Feb;109(1):64-8. Review. PubMed PMID: 22428450.
- The released CPP crystals enter the joint fluid. (Most joints are encapsulated by a delicate membrane, which produces lubricating joint fluid.) The loose crystals can then lodge in the surrounding soft joint tissue, such as the joint’s synovial lining, bursa, ligaments, and tendons.
- Once lodged in the joint’s soft tissue(s), the CPP crystals trigger an immune system response. This immune system response produces inflammation, pain, swelling, redness, and warmth, that may be diagnosed as either pseudogout or chronic CPP crystal inflammatory arthritis.
Because CCP crystals can be associated with metabolic and endocrine disorders, a health care provider may recommend a person diagnosed with CPPD disease be screened for these disorders. 6 Iqbal SM, Qadir S, Aslam HM, Qadir MA. Updated Treatment for Calcium Pyrophosphate Deposition Disease: An Insight. Cureus. 2019;11(1):e3840. Published 2019 Jan 7. doi:10.7759/cureus.3840
CPPD and joint damage
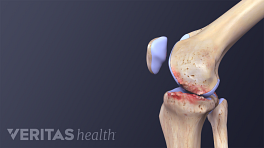
Repeated instances of pseudogout inflammation can permanently damage joints over time. Chronic CPP arthritis can also cause permanent joint damage. This damage is diagnosed as secondary osteoarthritis. (In contrast, idiopathic osteoarthritis has no known cause.)
Research suggests people who have osteoarthritis are up to three times more likely to have calcium pyrophosphate crystal deposits than those who do not. 7 Zhang et al. European League Against Rheumatism recommendations for calcium pyrophosphate deposition. Part I: terminology and diagnosis. Ann Rheum Dis. 2011 Apr;70(4):563-70. Epub 2011 Jan 7. PubMed PMID: 21216817. Whether the crystals cause joint damage or are the result of joint damage 8 Nalbant S., Martinez JAM, Kitumnuaypong T, Clayburne G, Sieck M, Schumacher HR. Synovial fluid features and their relations to osteoarthritis severity: new findings from sequential studies. Osteoarthritis and Cartilage 11, 50-54 (2003). —or both 9 Schuemacher HR, Chan LX, Zhang LY. Diagnosis of crystal associated diseases: Where do we stand? (Editorial) Bioanalysis. May 2011, Vol. 3, No. 10, Pages 1081-1083, DOI 10.4155/bio.11.75 —has long been debated. Scientists agree more research needs to be done in this area.
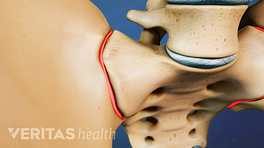
Chondrocalcinosis
Even people who have CPPD and no symptoms may eventually experience negative effects. CPPD is the leading cause of cartilage calcification. 7 Zhang et al. European League Against Rheumatism recommendations for calcium pyrophosphate deposition. Part I: terminology and diagnosis. Ann Rheum Dis. 2011 Apr;70(4):563-70. Epub 2011 Jan 7. PubMed PMID: 21216817. Calcification makes the cartilage harder and less flexible, and it is associated with osteoarthritis. 10 Brandt KD. Chondrocalcinosis, osteophytes and osteoarthritis. Annals of the Rheumatic Diseases 2003;62:499-500.
Doctors sometimes refer to cartilage calcification is called chondrocalcinosis. The process may occur in a seemingly healthy joint or a joint that has already had some degeneration.
- 1 Genetic and Rare Diseases Information Center, National Institute for Advancing Translational Sciences. Chondrocalcinosis 2. Last updated January 12, 2018. Accessed August 4, 2020. https://rarediseases.info.nih.gov/diseases/1292/chondrocalcinosis-2
- 2 Slobodonick A, Toprover M, Pillinger M. Crystal Arthritis. In: Efthimiou P, ed. Absolute Rheumatology Review. Springer Nature Switzerland AG; 2020; chap 15. Accessed September 15, 2020. https://doi.org/10.1007/978-3-030-23022-7_15
- 3 Viriyavejkul P, Wilairatana V, Tanavalee A, Jaovisidha K. Comparison of characteristics of patients with and without calcium pyrophosphate dihydrate crystal deposition disease who underwent total knee replacement surgery for osteoarthritis. (Abstract only.) Osteoarthritis Cartilage. 2007 Feb;15(2):232-5. Epub 2006 Oct 10. PubMed PMID: 17045495.
- 4 Pritzker KP. Crystal deposition in joints: prevalence and relevance for arthritis. J Rheumatol. 2008 Jun;35(6):958-9. PubMed PMID: 18528950.
- 5 Ivory D, Velázquez CR. The forgotten crystal arthritis: calcium pyrophosphate deposition. Mo Med. 2012 Jan-Feb;109(1):64-8. Review. PubMed PMID: 22428450.
- 6 Iqbal SM, Qadir S, Aslam HM, Qadir MA. Updated Treatment for Calcium Pyrophosphate Deposition Disease: An Insight. Cureus. 2019;11(1):e3840. Published 2019 Jan 7. doi:10.7759/cureus.3840
- 7 Zhang et al. European League Against Rheumatism recommendations for calcium pyrophosphate deposition. Part I: terminology and diagnosis. Ann Rheum Dis. 2011 Apr;70(4):563-70. Epub 2011 Jan 7. PubMed PMID: 21216817.
- 8 Nalbant S., Martinez JAM, Kitumnuaypong T, Clayburne G, Sieck M, Schumacher HR. Synovial fluid features and their relations to osteoarthritis severity: new findings from sequential studies. Osteoarthritis and Cartilage 11, 50-54 (2003).
- 9 Schuemacher HR, Chan LX, Zhang LY. Diagnosis of crystal associated diseases: Where do we stand? (Editorial) Bioanalysis. May 2011, Vol. 3, No. 10, Pages 1081-1083, DOI 10.4155/bio.11.75
- 10 Brandt KD. Chondrocalcinosis, osteophytes and osteoarthritis. Annals of the Rheumatic Diseases 2003;62:499-500.