Pain and swelling in a joint can be a sign of bursitis. The swelling may be significant, especially when the front of the knee or the tip of the elbow is affected. In other areas, such as the hip and shoulder, bursitis may cause pain without noticeable swelling.
Bursitis typically affects just one joint at a time. It has earned some interesting names over the years, such as housemaid’s knee, student’s elbow, and tailor’s bottom.
This article discusses what bursitis is, how it develops, what it feels like, how to treat it, and strategies to prevent it from flaring up.
In This Article:
- What Is Bursitis?
- Bursitis Treatment and Prevention
Bursitis Is Inflammation of a Bursa
When a bursa becomes inflamed, it is called bursitis. This inflammation can lead to uncomfortable symptoms and may negatively affect nearby tissues, such as tendons.
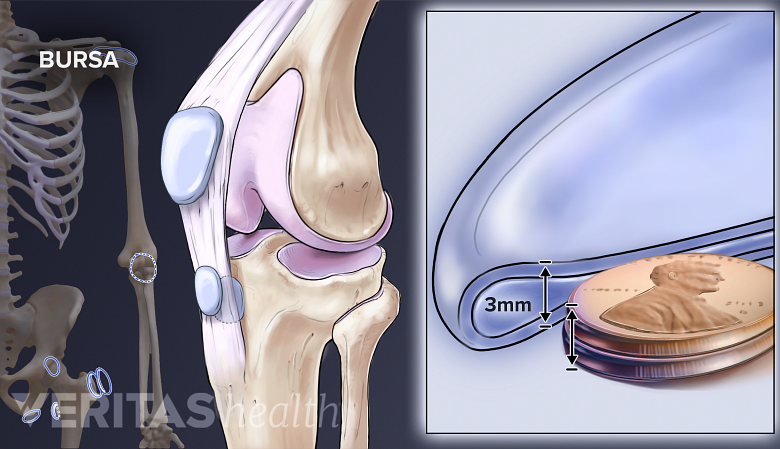
Bursa anatomy
Bursas are found near joints such as the elbow, knee, shoulder, and hip.
To understand bursitis, it helps to know a few key terms:
- A bursa is a small, thin, slippery sac filled with fluid. Bursae are located near joints, and they reduce friction between bone and surrounding soft tissue, such as skin, muscles, ligaments, and tendons.
- A bursa sac is made up of a delicate outer membrane, called a synovial membrane.
- Synovial fluid is produced by the synovial membrane. This viscous, lubricating fluid is contained in the bursa sac.
A bursa may be categorized by the tissue it lies next to. For example, a subcutaneous bursa can be found between a bone and skin (in Latin, cutaneous means relating to the skin) and a subtendinous bursa can be found between a bone and a tendon.
When inflamed, a bursa’s lining thickens and may produce too much synovial fluid, causing the bursa to swell. An inflamed, swollen bursa may be several times the size of a normal, healthy bursa.
What Causes Bursitis
There are several reasons a bursa may become inflamed. Typically, inflammation is related to irritation, friction, or trauma to a bursa:
- Excess irritation occurs when pressure is repeatedly put on the bursa. For example, repeatedly leaning on the elbows may lead to elbow bursitis, and wearing shoes that rub uncomfortably against the back of the foot may lead to heel bursitis.
- Excess friction can occur between the bursa and the nearby soft tissues. For example, during hip and knee movements a thick band of tissue called the iliotibial band (IT band) passes back and forth over the hip’s trochanteric bursa. If the IT band is too tight, walking or exercising may lead to excess friction and hip bursitis.
- A trauma can cause a bursa to temporarily fill with blood, causing swelling and irritation of the bursa’s synovial lining. For example, banging the kneecap on a hard surface may lead to knee bursitis.
Bursitis can also be associated with underlying medical conditions, particularly forms of inflammatory arthritis that cause changes to a joint, such as rheumatoid arthritis or gout.
Bursitis Symptoms
Unless bursitis is caused by an injury, the signs and symptoms usually develop gradually, over several days or weeks. The signs and symptoms may include:
- Swelling as the bursa fills with fluid
- Pain stemming from inflammation of the bursa and possible problems in nearby soft tissues
- Tenderness that is triggered when pressing the skin over the bursa
- Stiffness that limits the joint’s ability to comfortably bend and straighten
- Skin redness and warmth, which may be signs of skin irritation, bursal inflammation, or an infection. (A possible infection should be evaluated by a physician and treated immediately.)
Bursitis signs and symptoms can vary depending on several factors, including the severity of inflammation and its underlying cause. Another important factor is the bursa’s location:
- Visible swelling, skin redness, and skin warmth are more likely when the inflamed bursa is located directly under the skin. Bursae located just under the skin are called subcutaneous bursae. Examples of subcutaneous bursa include the prepatellar bursa at the front of the knee, the olecranon bursa at the tip of the elbow, and the subcutaneous calcaneal bursa at the back of the heel.
- Little or no visible swelling, skin redness, or skin warmth is more likely when the inflamed bursa is located under many layers of soft tissue. Examples of these types of bursae include the greater trochanteric bursa in the hip and the subacromial bursa in the shoulder.
A person’s anatomy can also affect whether or not swelling is noticeable. For example, a person who has excess weight or loose skin may not notice mild or moderate swelling in a knee or elbow.
Septic Bursitis
If the bursa is suspected to be infected, immediate medical attention is needed.
When a bursa is infected, it is called septic bursitis. This condition requires urgent medical care and treatment with antibiotics. While septic bursitis can develop in any bursa, it is most likely to occur in the prepatellar bursa at the front of the knee and the olecranon bursa at the tip of the elbow.
Signs and symptoms of septic bursitis
Certain physical signs are more likely to appear when a bursa is infected. These signs may affect the skin over the joint or the whole body.
The skin over the inflamed bursa may:
- Be red
- Feel warm to the touch 1 Smith DL, McAfee JH, Lucas LM, Kumar KL, Romney DM. "Septic and nonseptic olecranon bursitis. Utility of the surface temperature probe in the early differentiation of septic and nonseptic cases," (Abstract only) Arch Intern Med, 1989;149(7):1581-1585. PMID 2742432.
- Look patchy or have a rash, bumps, or sores (indicating a skin infection)
Septic bursitis can also cause body-wide symptoms, such as:
- Fever 2 García-Porrúa C, González-Gay MA, Ibañez D, García-País MJ. J Rheumatol. 1999 Mar; 26(3):663-7. As cited inBlackwell JR, Hay BA, Bolt AM, Hay SM. Olecranon bursitis: a systematic overview. Shoulder Elbow. 2014;6(3):182–190. doi:10.1177/1758573214532787.
- Fatigue
- A general feeling of being sick
Septic bursitis occurs when an infectious bacterium or other microorganism enters the bursa. These microorganisms may enter through a cut, scrape, puncture, bug bite, or other means. Sometimes an infection occurs without an obvious entry point on the skin.
Urgent medical care
Septic bursitis requires a prompt medical diagnosis and treatment with antibiotics. Failure to treat it quickly may cause septic bursitis to become chronic 3 Truong J, Mabrouk A, Ashurst JV. Septic Bursitis. [Updated 2020 Sep 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470331/?report=classic or may cause a life-threatening infection to develop.
Learn more about Septic Bursitis, including who is most likely to get it and how it is treated.
Bursitis Diagnosis
When a patient reports symptoms of bursitis, a doctor will perform a clinical examination and ask questions, such as when pain and swelling began. The doctor will consider other possible causes of the joint symptoms, such as arthritis and tendinitis.
Depending on the circumstances, a doctor may order medical imaging, such as an x-ray, MRI, or diagnostic ultrasound. The doctor may also recommend a procedure called bursal aspiration. This procedure involves removing fluid from the bursa using a needle and syringe, and it may be performed for diagnostic purposes, treatment, or both.
Read about Aspiration, the details of the procedure, and its potential benefits and risks.
If septic bursitis is suspected, lab tests may be ordered to confirm the presence of the infection.
What type of doctors diagnose and treat bursitis?
Many doctors are qualified to diagnose and make treatment recommendations for bursitis. Examples include:
- Primary care providers, such as family medicine doctors and internists
- Doctors who specialize in sports medicine
- Physiatrists
- Orthopedists
- Rheumatologists
- Podiatrists (for bursitis in the foot or ankle)
A doctor may refer a patient to another specialist depending on the patient’s unique health circumstances.
Read more about Arthritis Treatment Specialists
- 1 Smith DL, McAfee JH, Lucas LM, Kumar KL, Romney DM. "Septic and nonseptic olecranon bursitis. Utility of the surface temperature probe in the early differentiation of septic and nonseptic cases," (Abstract only) Arch Intern Med, 1989;149(7):1581-1585. PMID 2742432.
- 2 García-Porrúa C, González-Gay MA, Ibañez D, García-País MJ. J Rheumatol. 1999 Mar; 26(3):663-7. As cited inBlackwell JR, Hay BA, Bolt AM, Hay SM. Olecranon bursitis: a systematic overview. Shoulder Elbow. 2014;6(3):182–190. doi:10.1177/1758573214532787.
- 3 Truong J, Mabrouk A, Ashurst JV. Septic Bursitis. [Updated 2020 Sep 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470331/?report=classic