Most people suffer from an aching neck or back at some point in their lives. When pain and stiffness develop gradually and become chronic, osteoarthritis may be the cause.
Osteoarthritis of the spine is common with aging. It involves 1 Efthimiou, Petros. (2020). Absolute Rheumatology Review. 10.1007/978-3-030-23022-7. :
- Inflammation of the spine’s joints, which are called facet joints
- A breakdown of the cartilage in the facet joints
- Changes to the spine’s vertebrae, including the development of osteophytes, also called bone spurs
This osteoarthritic process usually occurs slowly, over years. The resulting pain, stiffness, and other symptoms may come and go or be constantly present. Spinal osteoarthritis can also cause referred and/or radiating pain, such as headaches caused by osteoarthritis in the neck or foot tingling caused by osteoarthritis in the lower back.
See How Arthritis Causes Back Pain
Spinal osteoarthritis is associated with other spine-related conditions, such as degenerative disc disease and/or spinal stenosis. This article discusses spinal osteoarthritis as well as the conditions associated with it.
Spine Anatomy and Facet Joints
To understand spinal osteoarthritis, it helps to understand a bit about the anatomy of the spine, including the spine’s facet joints. It is the facet joints that are directly affected by osteoarthritis.
- The spine is made up of 33 vertebrae that are stacked on top of each other.
- The vertebrae are separated by vertebral discs, which provide cushioning and act as shock absorbers.
- The back of each vertebra has two upper and two lower projections called articular processes.
- The articular processes form joints with the articular processes of the vertebrae located above and below. These joints are called facet joints.
- The facet joints help stabilize the spine and allow for the neck and back to bend and twist.
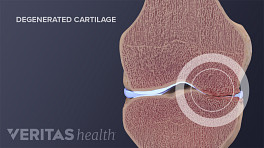
- Where facet’s surfaces meet, they are covered in slippery, smooth, flexible articular cartilage.
Articular cartilage allows the facets to move against each other without friction. The cartilage also acts as a shock absorber when the spine bears weight.
In This Article:
- What Is Spinal Osteoarthritis (Facet Joint Arthritis)?
- Spinal Osteoarthritis Symptoms
- Spinal Osteoarthritis Risk Factors
- Spinal Osteoarthritis Diagnosis
- Spinal Osteoarthritis Treatment
- Self Care and Exercise to Treat Spine Osteoarthritis
- Surgery for Spinal Osteoarthritis
- Lumbar Osteoarthritis Video
Facet joints are synovial joints
Health professionals classify facet joints as synovial joints. A delicate membrane, called a synovial membrane, encapsulates each facet joint. The membrane produces a viscous, slippery fluid, called synovial fluid that lubricates the joint.
Examples of other synovial joints include shoulders, elbows, knees, hips, and knuckles. All synovial joints are susceptible to osteoarthritis.
How Spinal Osteoarthritis Occurs
There are dozens of facet joints in the spine, and they are almost always in motion and bearing weight. Over time, everyday stress can wear down a facet joint’s cartilage, causing it to thin or disappear altogether.
In addition to daily wear and tear, other factors can also play a role in cartilage degradation, such as previous injuries to the joint, excess inflammation, and genetics.
Once a facet joint’s protective layer of cartilage is damaged or gone, the following process can occur:
- The facets’ bony surfaces may rub directly against each other, causing friction and inflammation.
- The inflammation may lead to changes in the joint’s soft tissues. For example, the facet joint’s synovial membrane may thicken and produce less viscous—and less lubricating—fluid.
- The friction may also cause the vertebral bones to produce excess tissue, resulting in bone spurs and/or enlarged joints.
- The excess bone tissue can cause more joint friction, leading to even more changes in the bone and surrounding soft tissues.
Certain areas of the spine are more susceptible to degeneration. These include the:
- Lower back, particularly the L4-L5 and L5-S1 segments of the lumbar spine 2 Basques BA, Espinoza Orías AA, Shifflett GD, et al. The Kinematics and Spondylosis of the Lumbar Spine Vary Depending on the Levels of Motion Segments in Individuals With Low Back Pain. Spine (Phila Pa 1976). 2017;42(13):E767‐E774. doi:10.1097/BRS.0000000000001967
- Neck, particularly the C5-C7 segments of the cervical spine 3 Moll LT, Kindt MW, Stapelfeldt CM, Jensen TS. Degenerative findings on MRI of the cervical spine: an inter- and intra-rater reliability study. Chiropr Man Therap. 2018;26:43. Published 2018 Oct 16. doi:10.1186/s12998-018-0210-2 , 4 Kuo DT, Tadi P. Cervical Spondylosis. [Updated 2020 May 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551557/?report=classic
The joints in the middle of the spine (thoracic spine) are less likely to develop painful osteoarthritis.
Vertebral discs and osteoarthritis
The vertebral discs can also degenerate over time. While health professionals and researchers know that vertebral disc degeneration and facet joint degeneration often occur together, they do not understand exactly how the degeneration of one structure influences the degeneration of another. 5 Bashkuev M, Reitmaier S, Schmidt H. Relationship between intervertebral disc and facet joint degeneration: A probabilistic finite element model study. J Biomech. 2020 Mar 26;102:109518. doi: 10.1016/j.jbiomech.2019.109518. Epub 2019 Nov 16. PubMed PMID: 31767286.
How Spine Osteoarthritis Causes Pain
Cartilage does not contain nerves, so damaged cartilage is not a source of pain. Likewise, bone spurs are normal signs of aging, and not necessarily a cause for concern. Rather, spine osteoarthritis can lead to pain because:
- Friction at the facet joints may lead to inflammation, which can cause pain.
- Muscle spasms may occur as a reaction to osteoarthritic changes. Muscle spasms can cause pain and stiffness and decrease function.
- Bone spurs and/or enlarged facet joints can impinge upon the spinal cord and nerve roots. This impingement can cause radicular symptoms and signs such as pain, tingling, and numbness in the areas supplied by the affected nerve.
- Other related changes, such as synovial cysts, may form near the facet joint capsules. Synovial cysts are abnormal but benign fluid-filled sacs. Like a bone spur, a synovial cyst can impinge on nerve roots.
Not everyone who has spine osteoarthritis feels symptoms. Researchers do not yet understand why some people experience arthritis pain and others do not.
When Spine Osteoarthritis Is Serious
Severe spinal osteoarthritis is typically accompanied by degenerative disc disease, spinal stenosis, or both. These conditions can lead to the compression of the spinal cord or its nerve roots, causing one or more of these symptoms:
- Excruciating lower back or neck pain that prevents most daily activity, including sleep
- Severe sharp, shooting, and burning pain in the leg(s) or arm(s)
- Progressive weakness in the leg(s) or arms(s)
- Numbness or tingling in the hands or feet
- Loss of bowel and/or bladder control (either inability to retain or release)
The loss of bowel and/or bladder control accompanied by one or more other symptoms may indicate a rare medical emergency called cauda equina syndrome. Urgent medical attention is crucial for making as full a recovery as possible.
Read more about Cauda Equina Syndrome on Spine-health.com
Osteoarthritis of the Spine: Many Names, One Disease
Osteoarthritis that develops in the spine can go by many different names, including:
- Facet joint arthritis
- Facet joint syndrome
- Facet arthropathy
- Zygapophyseal joint arthritis
- Z joint arthritis
It may also be referred to by terms that describe general degenerative changes in the spine, such as:
- Facet joint disorder, which refers to any disease of the facets, most commonly osteoarthritis
- Spondylosis, a general term that refers to any spine pain caused by degeneration, including but not limited to osteoarthritis
Regardless of the term used, spinal osteoarthritis is common. Experts estimate nearly everyone over the age of 60 shows signs of osteoarthritis in their spines, though not everyone experiences pain. 6 Eubanks JD, Lee MJ, Cassinelli E, Ahn NU. Does lumbar facet arthrosis precede disc degeneration? A postmortem study. Clinical Orthopaedics and Related Research 2007; 464:184-189. doi: 10.1097/BLO.0b013e3181583d4e As cited in Almeer G, Azzopardi C, Kho J, Gupta H, James SL, Botchu R. Anatomy and pathology of facet joint. J Orthop. 2020;22:109-117. Published 2020 Apr 8. doi:10.1016/j.jor.2020.03.058
- 1 Efthimiou, Petros. (2020). Absolute Rheumatology Review. 10.1007/978-3-030-23022-7.
- 2 Basques BA, Espinoza Orías AA, Shifflett GD, et al. The Kinematics and Spondylosis of the Lumbar Spine Vary Depending on the Levels of Motion Segments in Individuals With Low Back Pain. Spine (Phila Pa 1976). 2017;42(13):E767‐E774. doi:10.1097/BRS.0000000000001967
- 3 Moll LT, Kindt MW, Stapelfeldt CM, Jensen TS. Degenerative findings on MRI of the cervical spine: an inter- and intra-rater reliability study. Chiropr Man Therap. 2018;26:43. Published 2018 Oct 16. doi:10.1186/s12998-018-0210-2
- 4 Kuo DT, Tadi P. Cervical Spondylosis. [Updated 2020 May 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551557/?report=classic
- 5 Bashkuev M, Reitmaier S, Schmidt H. Relationship between intervertebral disc and facet joint degeneration: A probabilistic finite element model study. J Biomech. 2020 Mar 26;102:109518. doi: 10.1016/j.jbiomech.2019.109518. Epub 2019 Nov 16. PubMed PMID: 31767286.
- 6 Eubanks JD, Lee MJ, Cassinelli E, Ahn NU. Does lumbar facet arthrosis precede disc degeneration? A postmortem study. Clinical Orthopaedics and Related Research 2007; 464:184-189. doi: 10.1097/BLO.0b013e3181583d4e As cited in Almeer G, Azzopardi C, Kho J, Gupta H, James SL, Botchu R. Anatomy and pathology of facet joint. J Orthop. 2020;22:109-117. Published 2020 Apr 8. doi:10.1016/j.jor.2020.03.058